Research of the Freed-Pastor Lab
Our overall goal is to improve the lives of pancreatic cancer patients, with a particular focus on immune-based therapies.
Dissecting the mechanisms of immune evasion in pancreatic cancer
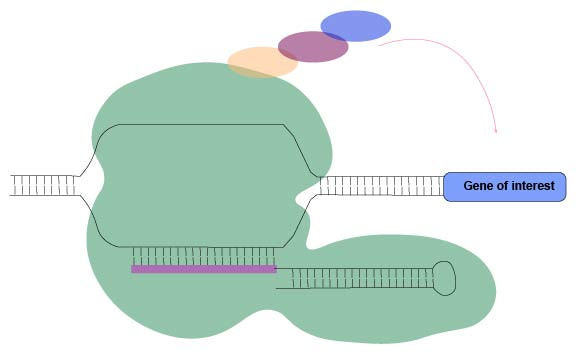
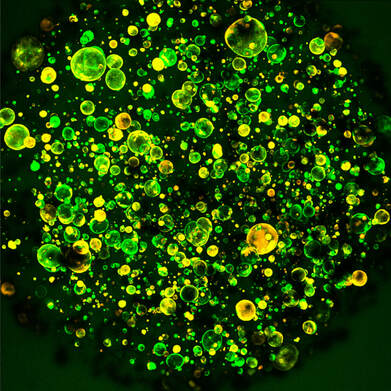
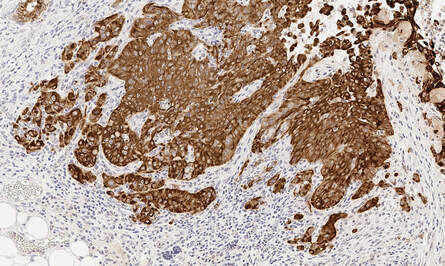
Pancreatic cancer is the third leading cause of cancer-related deaths in the United States. Despite considerable progress in understanding the molecular basis of this disease, pancreatic cancer continues to carry a dismal prognosis with fewer than 10% of patients surviving to five years. Decades of work has proven that the human immune system has the ability to recognize cancer as foreign, in a similar way to a virus or bacteria. However, cancers often acquire ways to “hide” from the immune system in order to avoid being killed. Insights into the mechanisms by which certain tumors “hide” from the immune system have fueled tremendous clinical successes in a range of tumor types. Unfortunately, the vast majority of pancreatic cancer patients have failed to benefit from current immune-based therapies. We use advanced preclinical modeling (organoids and mouse models) to investigate how pancreatic cancer escapes immune attack.
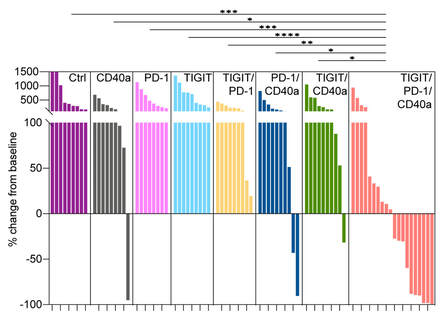
We recently developed preclinical models of “immunogenic” pancreatic cancer which facilitate the study of the interplay between a developing pancreatic tumor and the immune system with unprecedented detail. Using these mouse models, we have already uncovered a combination of three immunotherapy drugs (TIGIT/PD-1 co-blockade plus CD40 agonism; TIGIT/PD-1CD40a) that leads to profound responses in our preclinical models, now being evaluated as part of an early-phase clinical trial.
Pancreatic cancer is the third leading cause of cancer-related deaths in the United States. Despite considerable progress in understanding the molecular basis of this disease, pancreatic cancer continues to carry a dismal prognosis with fewer than 10% of patients surviving to five years. Decades of work has proven that the human immune system has the ability to recognize cancer as foreign, in a similar way to a virus or bacteria. However, cancers often acquire ways to “hide” from the immune system in order to avoid being killed. Insights into the mechanisms by which certain tumors “hide” from the immune system have fueled tremendous clinical successes in a range of tumor types. Unfortunately, the vast majority of pancreatic cancer patients have failed to benefit from current immune-based therapies. We use advanced preclinical modeling (organoids and mouse models) to investigate how pancreatic cancer escapes immune attack.
We recently developed preclinical models of “immunogenic” pancreatic cancer which facilitate the study of the interplay between a developing pancreatic tumor and the immune system with unprecedented detail. Using these mouse models, we have already uncovered a combination of three immunotherapy drugs (TIGIT/PD-1 co-blockade plus CD40 agonism; TIGIT/PD-1CD40a) that leads to profound responses in our preclinical models, now being evaluated as part of an early-phase clinical trial.
HOME | PEOPLE | RESEARCH | PUBLICATIONS | PROTOCOLS/REAGENTS | SUPPORT | CONTACT
©2022 Freed-Pastor Lab at Dana-Farber Cancer Institute
©2022 Freed-Pastor Lab at Dana-Farber Cancer Institute